|
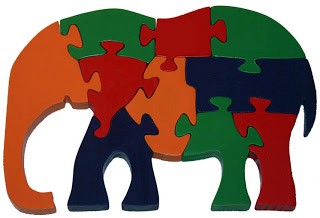
By Bart Magee, Ph.D. Why have we not cured mental illness? And more importantly, why is there no movement advocating for that goal? May is mental health awareness month which means it’s the month of the year when we see more discussion of the problems related to mental health than in any other. We will hear, again, that depression is the leading cause of disability worldwide, leaving billions of dollars in lost productivity, devastating pain, and death in its wake. We will read more stories of the harrowing struggles of individuals suffering in isolation. We will hear more calls for early detection, intervention, and increased awareness. What we won’t hear about is a strategy to fully address the problem. Despite billions of dollars of research and millions of pages of published study, not only do we lack a comprehensive theory of mental illness, but our current efforts to manage it are falling short, as rates of illness are rising. So it’s time for us to ask the hard question: What would it look like if mental illness were solved or “cured” and how can we make that happen? In the next few posts, I’d like to address that question. First, how did we get here? The best way to start would be to recall the parable of the blind men and the elephant. It is the story of a group of blind men, who have never come across an elephant before and who learn about the elephant by touching it. Each blind man feels a different part of the elephant’s body, but only one part, and he forms his impression based on that. In the parable, as with many problems that humans encounter, rather than thinking together and developing a concept of the whole of the elephant, they fight over whose version is correct. Is the elephant a rigid tusk, a wily trunk, or a big floppy ear? The same has been true in the study of mental illness. Throughout history there have been many approaches to the problem and all of them have had only limited results. Psychoanalysis, behaviorism, social psychology, biological psychiatry — each of these disciplines have addressed a narrow aspect of how the mind/brain/self can become “ill” and how to restore health. On their own, no single approach has come close to solving the problem and it’s not for lack of trying. We’ve gained vast knowledge from each perspective, from their successes and failures. As with the metaphor, each blind man has learned a tremendous amount about each part of the elephant’s body, but they all continue to be far too focused on discovering the absolute truth through a narrow lens and wasting time and energy on arguments and turf battles. It’s folly; people are dying; it needs to stop. We have all the pieces of the puzzle at hand. What we need to do is come together, think together, and make a collective effort to put it together.
Historically, the causes and treatments of mental illness have clustered around several core concepts. The etiology has been seen variously as supernatural, somatic, psychological, or social. The supernatural theory saw mental illness as caused by a displeasure of the gods, possession by evil spirits, or through sin. One of the earliest treatments for mental illness, trephination, sought to release evil spirits trapped within the skull by drilling holes in it. Fortunately, we’ve moved away from that and other such brutal methods, like chaining people to the walls of asylums, or burning people at the stake. While the supernatural approach has faded as a dominant theory today, we can still see its remnants in the way mental illness still can be seen as a moral failing and only managed through personal, spiritual struggle. On the one hand, this way of thinking has been rightly blamed for the continuing problem of shame and stigma around mental illness. On the other, the transformational potential of spiritual practices, including mediation and prayer, have been well documented. It is also important to emphasize that the capacity to find meaning in existence, to connect with values and a sense of purpose outside the self, are all foundations of mental well-being. The somatic model of mental illness also has a long history, starting with the ancient Egyptian and Greek theories of the wandering uterus. It took several millennia for this brazenly misogynistic idea to be wholly discarded, and during that time many other biological theories have come and gone. The somatic theory gained peak prominence and promise in the late 20th century with the rise of biological psychiatry. Prominence came through the discovery of the serotonin reuptake inhibitors (SSRIs), such as Prozac, which had marked effect on mood with relative safety and few side effects. This nourished the theory that all mental illnesses were caused by “chemical imbalances” that could be effectively treated with drugs. In the 1990’s, as a graduate student in psychology, I remember hearing from my professors the prediction that within a decade, psychologists would be primarily engaged in testing and diagnosis, as treatments would come in pill form. Not surprisingly, we saw a push for psychologists to gain prescription privileges. Today, the story couldn’t be more different. Biological approaches have hit a wall, as few new pharmacological treatments have been discovered and other biological therapies (i.e. brain stimulation) have had only narrow results. Updated theories of brain illnesses and genetic causes also fail to encompass the varied manifestations and courses of mental illness. At the same time, the study of the brain has yielded new understandings of how neurochemicals, brain connectivity, and bodily processes effect mood and behavior. Recently, studies have shown that psychoactive drugs like Ketamine and MDMA used in combination with psychotherapy are effective in treating depression, Post-Traumatic Stress Disorder (PTSD), and other maladies. In addition, Somatic Therapy, which combines talk therapy with various kinds of body-based interventions (movement, breathing, relaxation exercises) has shown promise in the treatment of diverse conditions from anxiety, to PTSD, and addiction. Out of nineteenth century Europe came the psychogenetic etiology of mental illness, which evolved to what we now know as Psychoanalysis. Sigmund Freud conceptualized symptoms and irrational behaviors as resulting from internal emotional conflicts which were largely unconscious. Freud’s “talking cure” found that making those conflicts conscious and putting words to repressed or dissociated experiences could relieve symptoms and restore health. At the same time that Freud and his followers were delving deep into the psyche, behaviorists were focusing on the manifestations of mental health problems as “maladaptive behaviors” and taking a learning theory approach to treatments. Out of these two traditions grew a multitude of talk therapies all competing for recognition and scientific support. Researchers and academics began rigorously studying psychotherapy and the search for “evidence-based” therapy began. The race is far from over and as it progresses, questions about epistemological bias and stealthy political agendas continue. The safe bets are on no winner emerging at all, which might be the best outcome for patients. The attention to finding the “gold standard” for therapy not only has privileged one-size-fits-all methods, but has neglected the fact that there has been tremendous innovation in psychotherapy treatment over the last few decades and the consensus of evidence points to the general effectiveness of therapy. Therapies that are grounded in the relationship or treatment alliance, are guided by a coherent formulation of the problem, utilize empathic methods for exploration, instill hope, create a structure for change, and integrate cultural and environmental factors, all have positive outcomes. The social perspective on mental illness traces its beginnings to the industrial revolution, whose effect created social problems that impacted individuals — unemployment, orphaned children, chronic disability, and poverty amid growing wealth and social inequality. In the mental health field, social work gained prominence in the mid-20th century and influenced mental health care around the time of the closing of the asylums and the development of community-based models of treatment. Social theories of mental illness locate mental health problems at the intersection between the individual and the social environment. Illness can be caused by a breakdown in the face of overwhelming environmental stress and can also be the result of problems in the broader organization of society. To the degree that power is unequally distributed in society, individuals suffer from various forms of oppression and injustice (i.e. racial discrimination and class oppression) which impact the individual’s mental health and behavior. Social workers attempt to address problems in systems and in the individual’s relationship to them. Their emphasis is on helping people who are the most disenfranchised socially, the least privileged among us. Compared to the biological and psychological approaches, the social perspective has been historically marginalized in the field of mental health, not unlike the populations served by social workers and case managers. Their work is often only minimally incorporated into the work of psychotherapists and psychiatrists which is ironic given that social workers provide more mental health services than all other mental health care providers combined. From this brief and condensed history, it’s clear that these divergent perspectives each hold important insights into the mental health elephant and if one steps back and takes a multifaceted view, an image of the whole animal begins to come into focus. At this point in history, very little has been done to encourage that kind of perspective-taking and real sharing of the deep knowledge gained from all of the various disciplines. If we are going to really solve mental illness we have to create a new path, one where collaboration and collective action animate our efforts. I’ll take up the question of what such a coordinated and comprehensive undertaking might look like in future posts.
2 Comments
8/28/2022 11:31:55 pm
Thank you for your kind words and for reminding us of the importance of seeking the right kind of help when we need it!
Reply
Your comment will be posted after it is approved.
Leave a Reply. |
Archives
April 2024
Categories |